Introduction
Introduction
Thank you for your interest in expanding the mental health workforce. The following describes the need, the possible solutions, and our project to help with the workforce shortage by up training providers in managing patients with mental health problems. Max Lydiatt, John Mitchell, and Bill Lydiatt are physicians with an interest in expanding the capacity of primary care, specialty care physicians, APPs, nurses, social workers, and others to increase their confidence and abilities in managing mild to moderate mental illness. This effort, called Bridges to Mental Health Workforce Expansion Project, required the help and guidance of many people. We are greatly indebted to so many for helping us develop this model. This site has many links to aid in diagnosis, treatment, finding critical resources, and how you may sign up to attend future training events.
Community Need
The COVID pandemic accelerated the already crescendoing prevalence of mental health issues. Across the United States, as in Nebraska and Iowa, rates of depression and anxiety have become a significant stressor for citizens, health care providers, and health systems. In the United States, 21% of adults experienced mental health issues in 2020 (52.9 million people). This represents 1 in 5 adults. 5.6% of U.S. adults experienced serious mental illness in 2020 (14.2 million people). The increase has many reasons, but the net result is a substantial shortage of appropriately trained healthcare providers. Omaha alone has seen wait times to be seen by a psychiatrist or psychologist extend to 8-12 weeks. Waitlists, extending past 300 people at Nebraska Medicine, create risk for citizens. COVID has further strained the workforce as many have left health care or reduced their hours due to their own health and fatigue.

The data above show a substantial difference in prevalence of depression across the United States. This may be due to relative differences in risk factors but, perhaps more likely, is due to a lack of diagnosis.
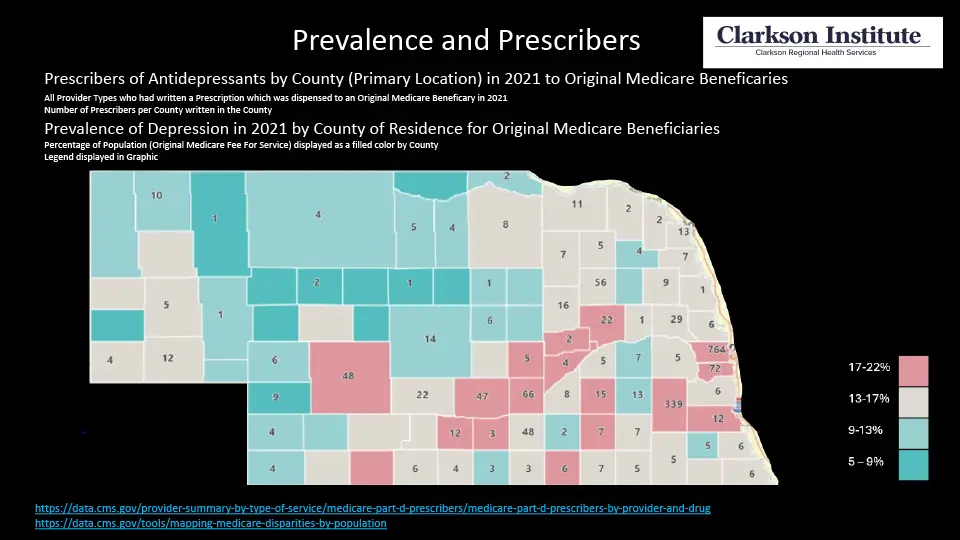
The same trend is seen in Nebraska. The relative prevalence of depression also tends to align with the number of providers available in a region. Lower prevalence of depression is seen in counties with few or no providers. Access is to diagnosis is a major hurdle.
There is a critical workforce shortage for mental health providers. Primary care and non-psychiatric specialists provide 80% of medical therapy for psychiatric issues. The workforce is inadequate to address the increasing burden of mental health issues. Psychiatrists are best suited to deal with those with severe mental illness, but that leaves up to 39 million Americans with mild to moderate mental illness (MMMI) on long wait lists while their symptoms worsen. People present to the emergency department in acute crises because they cannot be seen promptly through outpatient services. Emergency departments are an expensive and acute environment, not suited to treating someone with mild to moderate mental illness. Untreated mental illness increases hospital admission rates, making recovery much more complex and expensive. A growing sense of hopelessness, when untreated, increases the risk of suicide.
Through discussions with mental health leaders in the state, a review of needs assessment reports, and personal experience, we recognize workforce shortage is a significant impediment to improving mental health care in Nebraska. There are several ways to enhance the workforce in mental health. We need more individuals to go into the mental health field. This will require exposure at an early age while the individual’s career formation is still in its infancy. Improving lifestyle and benefits for existing mental health providers is also necessary to make students see this as a viable and rewarding career option. A third method is to expand the capacity of existing resources. This is the goal of Bridges to Mental Health.
The Bridges to Mental Health Workforce Expansion Project addresses this need by providing additional training and expertise for primary care and non-psychiatric specialists to expand the reach of psychiatrists through consultation with them.
Project Description
Bridges to Mental Health Workforce Expansion Project is an initiative supported by philanthropy to increase the behavioral health workforce in Nebraska. This novel project trains primary care, specialist physicians, advanced practice providers, nurses, and mental health workers. Physicians nearing the end of their practice or retired physicians wanting to stay involved and give back to the community are a second cohort we strive to reach.
The goal of this training will be to increase their diagnostic and therapeutic skills, confidence to expand their care, and heighten their awareness of common psychiatric disorders. The mental health training helps mitigate the access crisis by initiating early mental health treatment in areas where patients and the public already come for care. Retired physicians and APPs may be willing to help staff mental health clinics in existing or new spaces.
Specialists are treating patients with other health-related ailments who face various mental health issues, the origins of which or exacerbations are likely psychological or psychiatric in nature. These specialists, primary care physicians, advanced practice providers, and nurses are already seeing these patients but may be able to capitalize on the willingness of the patient to investigate all aspects of disease origin. Treating these patients with mild anxiety and depression that presents with these somatic complaints not only would improve patient care in these practices but also would limit the number of patients that go on to have more severe mental illness. In fact, there is evidence that patients that have somatic complaints tend to have more severe mental illness later in life. The goal is to achieve advanced training through a seminar with ongoing support and backup to this group of committed individuals.
For the individual participants, this study allows them to reflect on their current and future ability to care for patients with psychiatric illnesses and further solidify their knowledge of treating psychiatric conditions. The benefits are establishing a model for increasing the mental health workforce in Nebraska, thereby improving access and quality of care for patients while potentially reducing expensive acute care.
Partners & Collaborations
Our goal is to develop public, philanthropic, academic, and payor partnerships in our community. We have been fortunate to develop key initial partnerships as we have developed the program, including (in alphabetical order): Clarkson College; the Hawks Foundation; and The Nebraska Department of Health and Human Services Licensing Board of Medicine and Surgery. We are extremely grateful to our speakers, who hail from Massachusetts General Hospital Department of Psychiatry and the University of Vermont.
Results
So far, we have had seven cohorts totaling more than 400 participants from across Nebraska and Western Iowa.
Feedback has been overwhelming positive, underscoring the need for this expanded training. Pre- and post-surveys demonstrate a significant increase in rates of competence and confidence, showing the training is beneficial. These results were recently published in the medical journal Primary Care Companion.
Educational Resources and Guides
Click here to access:
- Common Rating Scales
- Integrated Healthcare Project, a grant-funded project at the Nebraska Medical Association in conjunction with Nebraska DHHS Division of Behavioral Health
- Kootenai Health Psychopharmacology Study Group-Behavioral Health Treatment Guidelines
- Omaha Community Resources, for a list of phone numbers and ideas for referrals
- Project PEACE (Psychiatric E-modules Advancing Clinician Education)
- Waco Guide to Psychopharmacology in Primary Care
Sign Up
- Register for upcoming sessions
- August 14-15, Kearney, NE
- August 18-19, Lauritzen Gardens, Omaha, NE
- November 6-7, Lincoln NE
- More information